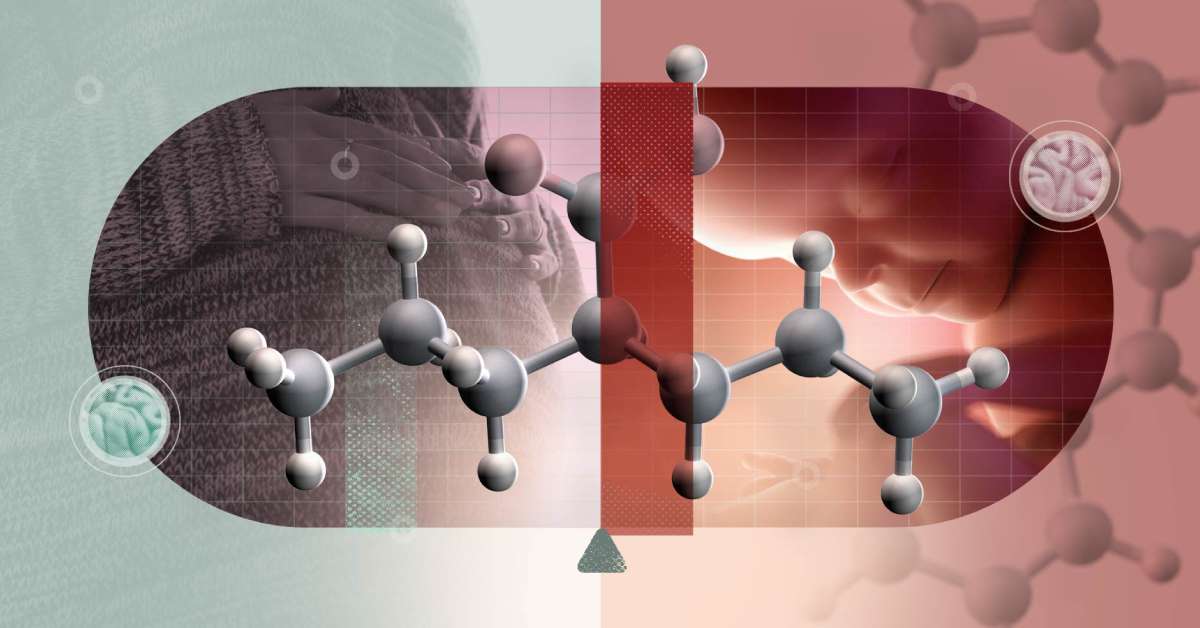
Access to antiseizure medication is improving in many parts of the world, but so are safety concerns. A new World Health Organization–commissioned study led by Dr Adrienne Chan and Professor Ian Wong from Aston University has revealed that global use of the drug valproate, while essential for epilepsy treatment, continues to rise despite its known risks to unborn babies.
Published in eClinicalMedicine (part of The Lancet Discovery Science), the study analysed antiseizure drug use across 73 countries between 2012 and 2022. Researchers found that although the expansion of treatment access is a positive step for neurological health, valproate remains the most widely prescribed medication, even though it can cause severe birth defects such as spina bifida and cleft palate, and lead to neurodevelopmental disorders affecting communication, memory, and behaviour.
The World Health Organization (WHO) includes valproate on its list of essential medicines but warns against prescribing it to women and girls of childbearing age due to these significant fetal risks. The agency has identified valproate-linked developmental disorders as a major global health concern.
According to Professor Wong and Dr Chan, this highlights a growing inequality in drug safety. While high-income countries have tightened regulations and introduced pregnancy prevention programmes that curb valproate prescriptions, low- and middle-income countries continue to rely on the drug due to limited availability and higher costs of newer antiseizure medications.
“Our findings show that access to antiseizure medicines is expanding globally, which is good news for patients who previously had little or no treatment options,” said Dr Chan. “But the continued widespread use of valproate in some parts of the world is concerning, given its known risks during pregnancy. Greater global alignment on safe prescribing and education is urgently needed to protect future generations.”
The research team emphasizes the need for urgent education campaigns and policy guidance to ensure that healthcare providers are aware of the risks and that safer alternatives are offered where possible. The next phase of their research will focus on prescription patterns within specific populations and on evaluating how effectively safety measures are implemented across regions.
The study’s findings underscore a critical public health message: access must go hand in hand with safety when it comes to essential medicines.